Blood glucose monitoring is a way of testing how much glucose is in the blood (glycemia).

i.)This is important in the care of diabetes mellitus. Most people with Type 2 diabetes need to test at least once per day (usually before breakfast) to assess the effectiveness of their diet and exercise for controlling their blood glucose levels. Many people with Type 2 are using an oral medication to combat their insulin resistance, and must test their blood glucose before and after breakfast to assess the effectiveness of their dosage.

ii.)All people who need to inject insulin, both for Type 1 diabetes and Type 2, need also to test their blood sugar more often (3 to 10 times per day) to assess the effectiveness of their prior insulin dose and to calculate their next insulin dose.
DIABETES MELLITUS TYPE 1
Diabetes mellitus type 1 (Type 1 diabetes, Type I diabetes, T1D, IDDM) is a form of diabetes mellitus. Type 1 diabetes is an autoimmune disease that results in the permanent destruction of insulin producing beta cells of the pancreas.

Type 1 is lethal unless treatment with exogenous insulin via injections replaces the missing hormone.

 DIABETES MELLITUS TYPE 2
DIABETES MELLITUS TYPE 2

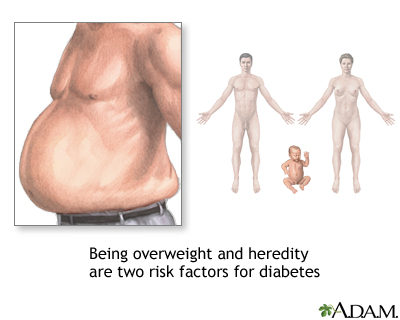
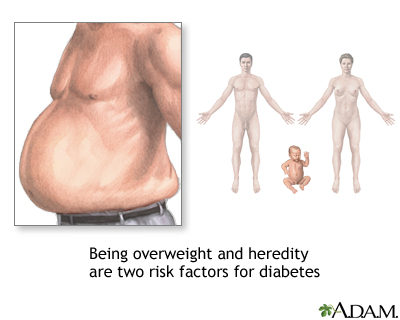
Diabetes mellitus type 2 (formerly called diabetes mellitus type II, non insulin-dependent diabetes (NIDDM), obesity related diabetes, or adult-onset diabetes) is a metabolic disorder that is primarily characterized by insulin resistance, relative insulin deficiency, and hyperglycemia.

It is often managed by engaging in exercise and modifying one's diet.

It is rapidly increasing in the developed world, and there is some evidence that this pattern will be followed in much of the rest of the world in coming years.
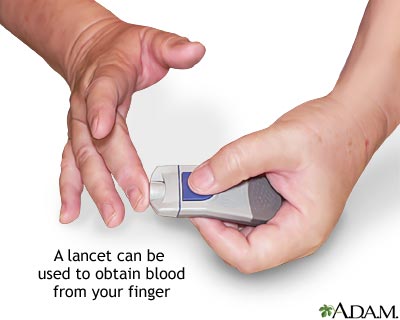
Improved technology for measuring blood glucose is rapidly changing the standards of care for all diabetic people. There are several methods of blood glucose testing currently available.
CHEMICAL TEST STRIPS Chemical test strips are a low cost method for monitoring blood glucose. A fairly large drop of blood, usually taken from the fingertip, is placed on a chemically prepared strip, called a blood glucose testing strip.The strip chemistry will cause it to change color according to the amount of glucose is in the blood.

One can tell if their level of blood glucose is low, high, or normal by comparing the color on the end of the strip to a color chart that is printed on the side of the test strip container.



These are recommended only for people who are occasionally monitoring their blood glucose level (prediabetic or type 2) and are not using insulin.
The Betachek Diabetes Test StripsBLOOD GLUCOSE METERS
A blood glucose meter is an electronic device for measuring the blood glucose level. A relatively small drop of blood is placed on a disposable test strip which interfaces with a digital meter. Within several seconds, the level of blood glucose will be shown on the digital display.
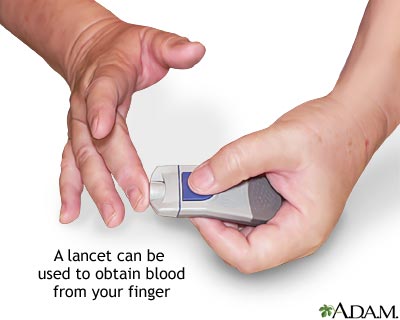


While more expensive, blood glucose meters seem a breakthrough in diabetes self care. As the drops of blood needed for the meter become smaller, the pain associated with testing is reduced and the compliance of diabetic people to their testing regimens is improved. Although the cost of using blood glucose meters seems high, it is believed to be a cost benefit relative to the avoided medical costs of the complications of diabetes.
A recent and welcome advance is the use of small blood drops for blood glucose testing from other places than the finger tips.

This alternate site testing uses the same test strips and meter, is practically pain free, and gives the real estate on the finger tips a needed break if they become sore.

(ALTERNATE SITE GLUCOSE TEST- BLOOD TAKEN FROM FOREARM INSTEAD OF FINGER)
CONTINUOUS BLOOD GLUCOSE MONITORING (AMBULATORY)A continuous blood glucose monitor determines blood glucose levels on a continuous basis (every few minutes). A typical system consists of:
i.)a disposable glucose sensor placed just under the skin, which is worn for a few days until replacement,

(A-INSULIN PUMP, B-CANNULA, C-TINY GLUCOSE SENSOR, D-REAL TIME TRANSMITTER)
ii.)a link from the sensor to a non-implanted transmitter which communicates to a radio receiver,

iii.)an electronic receiver worn like a pager (or insulin pump) that displays blood glucose levels on a practically continuous manner, as well as monitors rising and falling trends in glycemic excursions.


Continuous blood glucose monitors measure the glucose level of interstitial fluid. Disadvantages compared to traditional blood glucose monitoring are:
i.)continuous systems must be calibrated with a traditional blood glucose measurement (using current technology) and therefore do not yet fully replace "fingerstick" measurements.
ii.)glucose levels in interstitial fluid lag temporally behind behind blood glucose values.
Patients therefore require traditional fingerstick measurements for calibration (typically twice per day) and are often advised to use fingerstick measurements to confirm hypo- or hyperglycemia before taking corrective action.
The lag time discussed above has been reported to be about 5 minutes.Anecdotally, some users of the various systems report lag times of up to 10-15 minutes. This lag time is insignificant when blood sugar levels are relatively consistent. However, blood sugar levels, when changing rapidly, may read in the normal range on a CGM system while in reality the patient is already experiencing symptoms of an out-of-range blood glucose value and may require treatment. Patients using CGM are therefore advised to consider both the absolute value of the blood glucose level given by the system as well as any trend in the blood glucose levels. For example, a patient using CGM with a blood glucose of 100 mg/dl on their CGM system might take no action if their blood glucose has been consistent for several readings, while a patient with the same blood glucose level but whose blood glucose has been dropping steeply in a short period of time might be advised to perform a fingerstick test to check for hypoglycemia.
Continuous monitoring allows examination of how the blood glucose level reacts to insulin, exercise, food, and other factors. The additional data can be useful for setting correct insulin dosing ratios for food intake and correction of hyperglycemia. Monitoring during periods when blood glucose levels are not typically checked (e.g. overnight) can help to identify problems in insulin dosing (such as basal levels for insulin pump users or long-acting insulin levels for patients taking injections). Monitors may also be equipped with alarms to alert patients of hyperglycemia or hypoglycemia so that a patient can take corrective action(s) (after fingerstick testing, if necessary) even in cases where they do not feel symptoms of either condition. While the technology has its limitations, studies have demonstrated that patients with continuous sensors experience less hyperglycemia and also reduce their glycated hemoglobin levels.
Currently, continuous blood glucose monitoring is not automatically covered by health insurance in the United States in the same way that most other diabetic supplies are covered (e.g. standard glucose testing supplies, insulin, and even insulin pumps). However, an increasing number of insurance companies do cover continuous glucose monitoring supplies (both the receiver and disposable sensors) on a case-by-case basis if the patient and doctor show a specific need. The lack of insurance coverage is exacerbated by the fact that disposable sensors must be frequently replaced (sensors by Dexcom and Minimed have been FDA approved for 7- and 3-day use, respectively, though some patients wear sensors for longer than the recommended period) and the receiving meters likewise have finite lifetimes (less than 2 years and as little as 6 months). This is one factor in the slow uptake in the use of sensors that have been marketed in the United States.
Some current and future continuous glucose monitoring products include:
i.)
The Freestyle Navigatorii.)
Minimed Paradigm insulin pump plus a continuous sensoriii.)
The Guardian by Minimediv.)
Dexcom STSv.)
GlucoDay SSee this
summary by a diabetes support group for a review of CBGM products, performance, and features.
This technology is an important component in the effort to develop a closed-loop system connecting real-time automatic control of an insulin pump based on immediate blood glucose data from the sensor. One important goal is to develop an algorithm for automatic control, by which the system would function as an artificial pancreas. Although sensor reliability is more than adequate to improve outcomes for patients when used in an "open-loop" setting where the patient makes judgments about delivery of insulin, it is clearly not ready to be used as part of a closed loop system. FDA had approved the technology for use only in combination with fingerstick testing, and patients are expected to make judgments about treatment only after taking a fingerstick test. Therefore it is overly optimistic to think that these devices will be part of a closed loop system in the near future.
GLUCOSE SENSING BIOIMPLANTSLonger term solutions to continuous monitoring, not yet available but under development, use a long-lasting bio-implant. These systems promise to ease the burden of blood glucose monitoring for their users, but at the trade off of a minor surgical implantation of the sensor that lasts from one year to more than five years depending on the product selected.
Products under development include:
i.)
The SMSI Glucose Sensorii.)
The Animas Glucose Sensoriii.)
Implanted Glucose Bio-sensoriv.)
The Dexcom LTS (long term system)NON INVASIVE BLOOD GLUCOSE MONITORING TECHNOLOGYSome new technologies to monitor blood glucose levels will not require access to blood to read the glucose level. Non-invasive technologies include near IR detection, ultrasound and dielectric spectroscopy. These will free the person with diabetes from finger sticks to supply the drop of blood for blood glucose analysis.

Most of the non-invasive methods under development are continuous glucose monitoring methods and offer the advantage of providing additional information to the subject between the conventional finger stick, blood glucose measurements and over time periods where no finger stick measurements are available (i.e. while the subject is sleeping).

Products under development include:
i.)Fovioptics retinal glucose analyzer
ii.)
Inlight Solutions, NIR glucose sensoriii.)
NIR Diagnostics, NIR glucose sensoriv.)
Sinsys Medical GTSv.)
Solianis Monitoring AGVARIOUS MODELS OF MODERN GLUCOMETER



(COMBINED DIGITAL BP MONITOR & GLUCOMETER")

(ALTERNATE SITE TESTING GLUCOMETER)
SYMPTOMS,TESTS & ADVICE FOR DIABETIC PATIENTS1.)

2.)HYPERGLYCEMIA(HIGH BLOOD GLUCOSE) & HYPOGLYCEMIA (LOW BLOOD GLUCOSE) SYMPTOMS

(HYPERGLYCEMIA)


This method of treating low blood sugars is called the 15:15 rule. Eat 15 grams of carbohydrate and wait 15 minutes
3.)Fasting plasma glucose test -- this is the simplest and fastest way to measure blood glucose and diagnose diabetes. Fasting means that you have had nothing to eat or drink (except water) for 8 to 12 hours before the test. You are diagnosed with diabetes if your blood glucose level is 126 mg/dl or greater on two separate tests.

4.)Oral glucose tolerance test -- your blood glucose is tested two hours after drinking 75 grams of glucose. You are diagnosed with diabetes if your blood glucose level is 200 mg/dl or greater.


5.)A person with type 2 diabetes can use exercise to help control their blood sugar levels and provide energy their muscles need to function throughout the day. By maintaining a healthy diet and sufficient exercise, a person with type 2 diabetes may be able to keep their blood sugar in the normal non-diabetic range without medication.

(BEFORE & AFTER EXERCISES)
6.)RISKS OF DIABETES