i.)Radiography is the use of ionising electromagnetic radiation to view objects.
ii.)The modification of objects with radiation is not radiography. In cases of modification, when the object is a human or an animal and the purpose is a cure of disease, it is
radiotherapy and when the object is not living it could be
food irradation or some other form of
radiation processing.Diagnostic radiographyi.)Diagnostic radiography involves the use of both ionising radiation and non-ionising radiation to create images for medical diagnoses.
ii.)The predominant test is still the X-ray (the word X-ray is often used for both the test and the actual film or digital image). X-rays are the second most commonly used medical tests, after laboratory tests. This application is known as
diagnostic radiography. iii.)Since the body is made up of various substances with differing densities, X-rays can be used to reveal the internal structure of the body on film by highlighting these differences using attenuation, or the absorption of X-ray photons by the denser substances (like calcium-rich bones). Medical diagnostic radiography is undertaken by a specially trained professional called a diagnostic radiographer or a radiologic technologist in Healthcare centers.
SUB-SPECIALITIES OF DIAGNOSTIC RADIOGRAPHY :
a.)Projection radiography
b.)Fluoroscopy (angiography, gastro-intestinal fluroscopy)
c.)Dual energy X-ray absorptiometry
d.)Computed tomography
a.)
PROJECTION RADIOGRAPHYThe creation of images by exposing an object to X-rays or other high-energy forms of electromagnetic radiation and capturing the resulting remnant beam (or "shadow") as a latent image is known as "
projection radiography." The "shadow" may be converted to light using a fluorescent screen, which is then captured on photographic film, it may be captured by a phosphor screen to be "read" later by a laser (CR), or it may directly activate a matrix of solid-state detectors (DR--similar to a very large version of a CCD in a digital camera). Bone and some organs (such as lungs) especially lend themselves to projection radiography. It is a relatively low-cost investigation with a high diagnostic yield.
Projection radiography uses X-rays in different amounts and strengths depending on what body part is being imaged:
i.)
HARD TISSUESHard tissues such as bone require a relatively high energy photon source, and typically a tungsten anode is used with a high voltage (50-150 kVp) on a 3-phase or high-frequency machine to generate braking radiation. Bony tissue and metals are denser than the surrounding tissue, and thus by absorbing more of the X-ray photons they prevent the film from getting exposed as much. Wherever dense tissue absorbs or stops the X-rays, the resulting X-ray film is unexposed, and appears translucent blue, whereas the black parts of the film represent lower-density tissues such as fat, skin, and internal organs, which could not stop the X-rays. This is usually used to see bony fractures, foreign objects (such as ingested coins), and used for finding bony pathology such as osteoarthritis, infection (osteomyelitis), cancer (osteosarcoma), as well as growth studies (leg length, achondroplasia, scoliosis, etc).
ii.)SOFT TISSUES
Soft tissues are seen with the same machine as for hard tissues, but a "softer" or less-penetrating X-ray beam is used. Tissues commonly imaged include the lungs and heart shadow in a chest X-ray, the air pattern of the bowel in abdominal X-rays, the soft tissues of the neck, the orbits by a skull X-ray before an MRI to check for radiopaque foreign bodies (especially metal), and of course the soft tissue shadows in X-rays of bony injuries are looked at by the radiologist for signs of hidden trauma (for example, the famous "fat pad" sign on a fractured elbow).
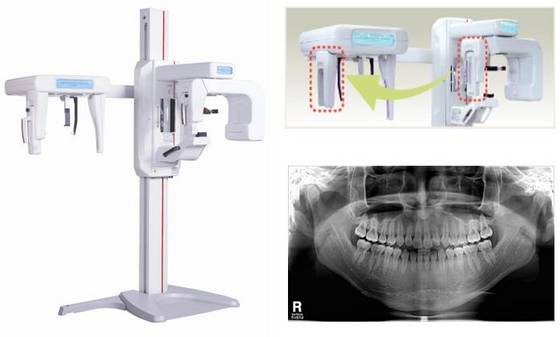
iii.)DENTAL RADIOGRAPHY
Dental radiography uses a small radiation dose with high penetration to view teeth, which are relatively dense. A dentist may examine a painful tooth and gum using X-ray equipment. The machines used are typically single-phase pulsating DC, the oldest and simplest sort. Dental technicians or the dentist may run these machines-- radiologic technologists are not required by law to be present.
iv.)MAMMOGRAPHY
Mammography is an X-ray examination of breasts and other soft tissues. This has been used mostly on women to screen for breast cancer, but is also used to view male breasts, and used in conjunction with a radiologist or a surgeon to localise suspicious tissues before a biopsy or a lumpectomy. Breast implants designed to enlarge the breasts reduce the viewing ability of mammography, and require more time for imaging as more views need to be taken. This is because the material used in the implant is very dense compared to breast tissue, and looks white (clear) on the film. The radiation used for mammography tends to be softer (has a lower photon energy) than that used for the harder tissues. Often a tube with a molybdenum anode is used with about 30 000 volts (30 kV), giving a range of X-ray energies of about 15-30 keV. Many of these photons are "characteristic radiation" of a specific energy determined by the atomic structure of the target material (Mo-K radiation).
b.)FLUOROSCOPY (angiography, gastro-intestinal fluroscopy)
Fluoroscopy is a term invented by Thomas Edison during his early X-ray studies. The name refers to the fluorescence he saw while looking at a glowing plate bombarded with X-rays.
This is a technique that provides moving projection radiographs of lower quality.
Fluoroscopy is mainly performed to view movement (of tissue or a contrast agent), or to guide a medical intervention, such as angioplasty, pacemaker insertion, or joint repair/replacement. The latter are often carried out in the operating theatre, using a portable fluoroscopy machine called a C-arm. It can move around the surgery table and make digital images for the surgeon.
Angiography is the use of fluoroscopy to view the cardiovascular system. An iodine-based contrast is injected into the bloodstream and watched as it travels around. Since liquid blood and the vessels are not very dense, a contrast with high density (like the large iodine atoms) is used to view the vessels under X-ray. Angiography is used to find aneurysms, leaks, blockages (thromboses), new vessel growth, and placement of catheters and stents. Balloon angioplasty is often done with angiography.
Fluoroscopy can be used to examine the digestive system using a substance which is opaque to X-rays, (usually barium sulphate or gastrografin), which is introduced into the digestive system either by swallowing or as an enema. This is normally as part of a double contrast technique, using positive and negative contrast. Barium sulfate coats the walls of the digestive tract (positive contrast), which allows the shape of the digestive tract to be outlined as white or clear on an X-ray. Air may then be introduced (negative contrast), which looks black on the film. The barium meal is an example of a contrast agent swallowed to examine the upper digestive tract. Note that while soluble barium compounds are very toxic, the insoluble barium sulfate is non-toxic because its low solubility prevents the body from absorbing it.
A number of substances have been used as positive contrast agents: silver, bismuth, cesium, thorium, tin, zirconium, tantalum, tungsten and lanthanide compounds have been used as contrast agents. The use of thoria (thorium dioxide) as an agent was rapidly stopped as thorium causes liver cancer.
Most modern injected radiographic positive contrast media are iodine-based. Patients who suffer from allergy to shellfish may be allergic to iodine, and should consult their physician regarding pre-medication to lessen risk of allergic reaction. Iodinated contrast comes in two forms: ionic and non-ionic compounds. Non-ionic contrast is significantly more expensive than ionic (approximately three to five times the cost), however, non-ionic contrast tends to be safer for the patient, causing fewer allergic reactions and uncomfortable side effects such as hot sensations or flushing. Most imaging centers now use non-ionic contrast exclusively, finding that the benefits to patients outweigh the expense.
Negative radiographic contrast agents are air and carbon dioxide (CO2). The latter is easily absorbed by the body and causes less spasm. It can also be injected into the blood, where air absolutely cannot.
c.)
Dual energy X-ray absorptiometryDEXA, or bone densitometry, is used primarily for osteoporosis tests. It is not projection radiography, as the X-rays are emitted in 2 narrow beams that are scanned across the patient, 90 degrees from each other. Usually the hip (head of the femur), lower back (lumbar spine) or heel (calcaneum) are imaged, and the bone density (amount of calcium) is determined and given a number (a T-score). It is not used for bone imaging, as the image quality is not good enough to make an accurate diagnostic image for fractures, inflammation etc. It can also be used to measure total body fat, though this isn't common. The radiation dose received from DEXA scans is very low, much lower than projection radiography examinations.
d.)
Computed tomographyComputed tomography or CT scan (previously known as CAT scan, the "A" standing for "axial") uses a high amount of ionizing radiation (in the form of X-rays) in conjunction with a computer to create images of both soft and hard tissues. These images look as though the patient was sliced like bread (thus, "tomography"-- "tomo" means "slice"). The machine looks similar to an MRI machine to many patients, but is not related. The exams are generally short, most lasting only as long as a breath-hold. Contrast agents are often used, depending on the tissues needing to be seen. Radiographers perform these examinations, sometimes in conjunction with a radiologist (for instance, when a radiologist performs a CT-guided biopsy).
Other TestsOther tests are often found within the radiology department, due to the fact that they are all diagnostic imaging (finding disease via imagery), but do not use ionising radiation (and thus are not technically radiography). As the dangers of ionising radiation are well known, other methods of imaging were sought out and have developed over the years. These are summarised below.
Nuclear medicineNuclear medicine is a speciality using injected or inhaled radioactive isotopes to image the body. Instead of passing ionising radiation through the patient, the patient becomes temporarily radioactive and is placed near gamma cameras, which detect the radioactivity and store it as an image. Images made with nuclear medicine is usually physiological, not anatomical; that is, the images show function quite well, but not anatomic structure. Examples of nuclear medicine tests are PET and SPECT. Tests are most often made of the heart, thyroid gland, and cancer studies. In veterinary use, scintigraphy is commonly used for diagnosing occult bone fractures and other bony pathology in horses. Nuclear Medicine Technologists in the United States registered by the ARRT (American Registry of Radiologic Technologists) and/or certified by the NMTCB (Nuclear Medicine Technology Certification Board) perform these examinations.
Medical ultrasoundUltrasound or sonography uses high frequency sound to create images. It is usually used to image the soft tissues of the abdomen, the pelvic area, the breasts, and the cardiovascular system, though it is also often used for guiding needles when doctors perform thoracentesis, amniocentesis, or biopsies. A specialised type of sonography is echocardiography, which specifically views the heart and surrounding major blood vessels. It has a well developed specialist training scheme, with postgraduate qualification, but is not recognised as its own profession by the Health Professions Council in the UK. Practitioners are most commonly registered diagnostic sonographers (US), radiographers (UK), doctors and midwives.
Magnetic resonance imaging (MRI)Also known as Nuclear Magnetic Resonance (NMR) in chemistry, this is another speciality of radiography that uses non-ionising radiation, in this case magnetic fields and radio frequencies, to create images. Most lay people tell this machine apart from CT by the long exam times (several minutes to an hour), the claustrophobic tunnel, and the loud pounding noise created by the growing and collapsing of the magnetic fields. Specially trained radiographers carry out these examinations. Post-graduate training is necessary to practice in this field for several reasons. The physics of MRI are slightly different and quite a bit more complex than in traditional (plain-film/screen, CR, DR) or even CT imaging modalities. Sectional soft tissue details when using MR have a different appearance than those in CT, requiring additional training to allow the technologist to become familiar with the appearances of both normal and pathologic anatomy which may require adjustment of technique. Finally the risk of serious injury to the patient far surpasses any such risk present in other imaging modalities. Magnetic field strength in medical MRI scanners range from 1.5 to 3 teslas on average. These fields would easily turn any ferromagnetic object into a projectile (this includes some necklaces, earrings, surgical pins, etc.) thus as the person actually conducting the examination, the technologist must ensure and be familiar with a full medical history to rule out implanted ferromagnetic objects, as well as (of course) ensuring no such objects (implanted or otherwise) enter the room with the patient. Although this may not seem like a difficult task, this risk of serious injury or death is very real, making this a major professional responsibility.
Radiotherapy and therapeutic radiographyAs part of the planning and execution of radiotherapy radiography is often used as part of the treatment of cancer in oncology departments, with 6 out of 10 patients treated with radiotherapy for cancer cured. This involves application of a prescribed dose of ionising radiation to specific targeted tissue, whilst limiting damage to the surrounding healthy area.
This treatment is prescribed by an oncologist and is conducted by radiotherapists, who are a group of professions working together, including medical physicists, therapy radiographers, and technicians.