MEDICAL IMAGING PROJECTS
MR Imaging
1.) Hyperpolarized Gas Polarimetry and Imaging at Low Magnetic Field
2.) Development of a Low-Field 3He MRI System to Study Posture-Dependence of Pulmonary Function
3.) Non-invasive assessment of regional ventilation in the human lung using oxygen-enhanced magnetic resonance imaging
4.) Spline Based Deformable Registration of MR Images
5.) A Complete Digital Magnetic Resonance Imaging (MRI) System at Low Magnetic Field (0.1 Tesla)
6.) NMR Hardware and Desktop Systems
7.) 3D Variational Brain Tumor Segmentation using a High Dimensional Feature Set
8.) 3D Visualisation of MRI images using MATLAB
9.) Contour Profiling of Brain Tumor Areas by Using Image Correlation and Peak Detection Techniques
10.) Automatic Detection & volume Determination Of Metastatic Brain Tumors
11.) Processing of visual stimuli in the brain: Investigations using simultaneous functional magnetic resonance imaging and electrophysiological recording.
12.) Efficient Multi-Modal Least-Squares Alignment of Medical Images Using Quasi-Orientation Maps
13.) Uniformity Correct ion with Homomorphic Filtering on Region of interest in MR imaging
14.) Quantification of Small Cerebral Ventricular Volume Changes in Treated Growth Hormone Patients Using Nonrigid Registration
15.) DEVELOPMENT OF ULTRA LOW-FIELD MAGNETIC RESONANCE IMAGING SYSTEM
16.) Ultra High Field MRI Whole-Slice and Localized RF Field Excitations Using the Same RF Transmit Array
17.) A MEDICAL IMAGE ENHANCEMENT ALGORITHM BASED ON TOPOLOGICAL DERIVATIVE AND ANISOTROPIC DIFFUSION
18.) Using MATLAB to Produce 3D Models, Segment CT and MRI Data, and Investigate Properties of Anatomical Volumes
CT / X-RAY IMAGING
1.) Registration of 3D angiographic and X-ray images using Sequential Monte Carlo sampling
2.) Three-dimensional Representation of the Human Arterial Tree
3.) Direct-Conversion Flat-Panel X-Ray Image Sensors for Digital Radiography
4.) Tumor Detection in the Bladder Wall with a Measurement of Abnormal Thickness in CT Scans
5.) Non-rigid registration methods assessment of 3D CT images for head- neck radiotherapy
6.) Computer-Aided Detection of Kidney Tumor on Abdominal Computed Tomography Scans
7.) Pulmonary nodule detection using chest CT images
8.) Computer aided diagnosis system for lung cancer based on helical CT images
9.) Contrast enhancement of soft tissues in Computed Tomography images
10.) Blind deblurring of CT images
BREAST IMAGING
1.) Breast Surface Estimation for Radar-Based microwave Breast Imaging Systems
2.) Estimating the breast surface using UWB microwave monostatic backscatter measurements
3.) Computer aided diagnostic systems for digital mammograms
4.) A combined system for detecting masses in mammographic images
5.) Detection of Breast Lesions in Medical Digital Imaging Using Neural Networks
6.) Computerized classification of suspicious regions in chest radiographs using subregion hotelling observers
7.) Computer Aided Diagnosis in Digital Mammograms: Detection of Micro-calcifications by Meta Heuristic Algorithms
8.) Analysis of Mammographic Micro-Calcifications Using Grey-Level Image Structure Features.
9.) Analysis of Asymmetry Mammograms via Directional Filtering With Gabor Wavelets
10.) Automatic identification of pectoral muscles in mammograms
11.) A fuzzy – genetic approach to breast cancer diagnosis
12.) Mammogram Image Size Reduction Using 16-8 bit Conversion Technique
13.) A Reconstruction Algorithm for Breast Cancer Imaging With Electrical Impedance Tomography in Mammography Geometry
14.) Measurement of Patient Exposure Dose on X-Ray Screening Mammography
Cardiac Imaging
1.) Multiresolution Approach for Non-Contact Measurements of Arterial Pulse using Thermal Imaging
2.) Automatic View Recognition for Cardiac Ultrasound Images
3.) Methods for Evaluating Left Ventricular Function Computed from ECG-Gated myocardial Perfusion SPECT
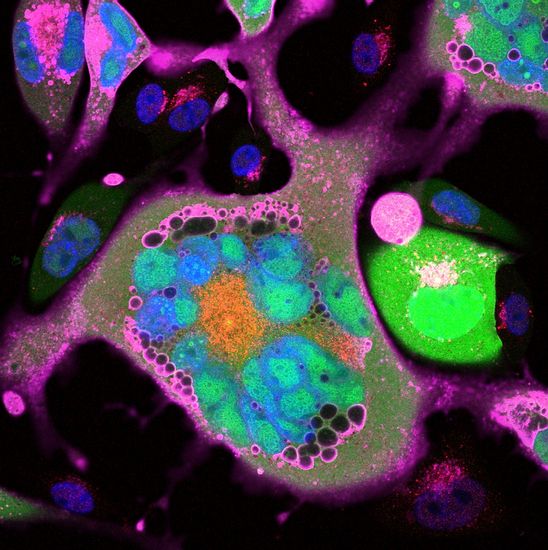
CELL IMAGING
1.) Cell Detections and Tracking Based on Bayesian Estimation Techniques in Biotechniques
2.) Early detection of lung cancer using 3D cell – CT
3.) Blur elimination of cell images with soft X-ray projection CT microscope
4.) An Image Mining Approach for Measuring Intensity, Size and Geographical localization of Stained Bodies in Cultured Cells: Application in Apoptosis Detection
IMAGE COMPRESSION & TRANSMISSION
1.) Efficient Image Compression of Medical Images Using the Wavelet
Transform and Fuzzy c-means Clustering on Regions of Interest.
2.) Compression of Medical Image Stacks using Wavelets and Zero-Tree Coding
3.) PARALLELIZATION OF HYPERSPECTRAL IMAGING CLASSIFICATION AND DIMENSIONALITY REDUCTION ALGORITHMS
Neuro-Imaging
1.) A feature-based approach to combine functional MRI, structural MRI and EEG brain imaging data
2.) A Method for Multi-Task FMRI Data Fusion Applied to Schizophrenia
3.) Analysis of FMRI Data by Blind Separation Into Independent Spatial Components
4.) Application of Independent Component Analysis to Magnetic Resonance Imaging for Enhancing the Contrast of Gray and White Matter
5.) Non-invasive Imaging of Cerebral Activation with Diffuse Optical Tomography
ELECTRICAL IMPEDANCE TOMOGRAPHY
1.) Electrical impedance tomography imaging using a priori ultrasound data
2.) Design of a modular adaptive Electrical impedance tomography system
3.) Image Reconstruction Methods for Electrical Impedance Tomography (EIT) on SUT-1 system
4.) 3-D Electrical Impedance Tomography of the human thorax
5.) A 32-electrode data collection system for Electrical Impedance Tomography
6.) Weighted Regularisation in Electrical Impedance Tomography with Applications to Acute Cerebral Stroke
7.) Kalman Filter Approach to track fast impedance changes in Electrical Impedance Tomography
8.) Regularized Reconstruction in Electrical Impedance Tomography using a variance Uniformization constant
9.) Krylov subspace Iterative techniques: On the Detection of brain activity with Electrical Impedance Tomography
EYE IMAGING
1.) Automatic diagnosis of diabetic retinopathy using fundus images
2.) Automated depth analysis of optic nerve head from stereo fundus images
3.) Digital Stereo Image Analyzer for Generating Automated 3-D Measures of Optic Disc
Deformation in Glaucoma
4.) Digital stereo-optic disc image analyzer for monitoring progression of glaucoma
5.) Design of an Automated Glaucoma Diagnostic System
6.) Automated method for fundus image registration and analysis
7.) Automatic 3D-Reconstruction of the Ocular Fundus from Stereo Images (3-d digital surface recovery of the optic nerve head from stereo fundus images)
8.) Retinal Vessel Extraction Using Multiscale Matched Filters, Confidence and Edge Measures
9.) Rapid automated tracing and feature extraction from live high-resolution retinal fundus images using direct exploratory algorithms
10.) Retinal thickness measurements from optical coherence tomography using a markov boundary model
11.) In vivo human retinal imaging by Fourier domain optical coherence tomography
12.) In vivo high-resolution video-rate spectral-domain optical coherence tomography of the human retina and optic nerve
13.) Early Detection on the Condition of Pancreas Organ as the Cause of Diabetes Mellitus by Real Time Iris Image Processing
14.) Segmentation of Medical Images using Fuzzy Mathematical Morphology
15.) Segmentation of Retinal Vasculature Using Wavelets and Supervised Classification
16.) High-Resolution In Vivo Imaging of the RPE Mosaic in Eyes with Retinal Disease
17.) In-vivo imaging of the photoreceptor mosaic in retinal dystrophies and correlations with visual function
THERMOGRAPHY IMAGING
1.) Forehead Thermal Signature Extraction in Lie Detection
2.) A Novel Approach for a Non-Invasive Diagnostic Technique of thyroid glands using thermographic systems
3.) A Correction Method of Medical Thermography's Distortion
4.) Application of Thermography for Non-Invasive Diagnosis of Thyroid Gland Disease
5.) Infrared thermography in the detection and management of coronary artery disease
6.) Automatic Feature Localization in Thermal Images for Facial Expression
Recognition
7.) ESTIMATION OF CORONARY BLOOD FLOW BY CARDIAC THERMOGRAPHY
IN OPEN CHEST CONDITIONS
8.) Non-contact, Wavelet-based Measurement of Vital Signs using Thermal Imaging
9.) PROCESSING THERMAL IMAGES TO DETECT BREAST CANCER AND ASSESS PAIN / EARLY BREAST CANCER DETECTION USING INFRARED IMAGING
10.) Thermal Image Analysis
for Polygraph Testing
11.) Thermal monitoring of the myocardium under blood arrest
12.) Multiresolution Approach for Non-Contact Measurements of Arterial Pulse using Thermal Imaging
US IMAGING
1.) Quantification of Thyroid Volume using 3-D ultrasound imaging
2.) Denoising images with wavelets: Modelling the backscatter noise in ultrasound images of tendons in limbs
3.) Parallel Computing in Time-Frequency Distributions for Doppler Ultrasound Blood Flow Instrumentation
4.) Identification of Vulnerable Atherosclerotic Plaque Using IVUS-Based Thermal Strain
Imaging
5.) Automatic boundary identification in ultrasound images of the prostate
6.) SPECKLE DETECTION IN ULTRASOUND IMAGES USING FIRST ORDER STATISTICS
7.) Ultrasound Image Segmentation by Using Wavelet Transform and Self-
Organizing Neural Network
8.) Breast Cancer Diagnosis Using Self-Organizing Map For Sonography
9.) Speckle Reduction in Ultrasonic Images of Atherosclerotic Carotid Plaque
10.) Fuzzy Neural Network Computer Assisted Characterization of Diffused Liver Diseases Using Image Texture Techniques on Ultrasonic Images
11.) Nonlinear analysis of carotid artery echographic images
12.) OVARIAN ULTRASOUND IMAGE ENHANCEMENT BY PSEUDOCOLORING
13.) SEGMENTATION OF PROSTATE CONTOURS FROM ULTRASOUND IMAGES