Fluoroscopy
Fluoroscopy is an imaging technique commonly used by physicians to obtain real-time images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an x-ray source and fluorescent screen between which a patient is placed. However, modern fluoroscopes couple the screen to an x-ray image intensifier and CCD video camera allowing the images to be played and recorded on a monitor. The use of x-rays, a form of ionizing radiation, requires that the potential risks from a procedure be carefully balanced with the benefits of the procedure to the patient. While physicians always try to use low dose rates during fluoroscopy procedures, the length of a typical procedure often results in a relatively high absorbed dose to the patient. Recent advances include the digitization of the images captured and flat-panel detector systems which reduce the radiation dose to the patient still further.
Fluoroscope designThe first fluoroscopes consisted of an x-ray source and fluorescent screen between which the patient would be placed. As the x rays pass through the patient, they are attenuated by varying amounts as they interact with the different internal structures of the body, casting a shadow of the structures on the fluorescent screen. Images on the screen are produced as the unattenuated x rays interact with atoms in the screen through the photoelectric effect, giving their energy to the electrons. While much of the energy given to the electrons is dissipated as heat, a fraction of it is given off as visible light, producing the images. Early radiologists would adapt their eyes to view the dim fluoroscopic images by sitting in darkened rooms, or by wearing red adaptation goggles.
X-ray Image IntensifiersThe invention of X-ray image intensifiers in the 1950s allowed the image on the screen to be visible under normal lighting conditions, as well as providing the option of recording the images with a conventional camera. Subsequent improvements included the coupling of, at first, video cameras and, later, CCD cameras to permit recording of moving images and electronic storage of still images.
Modern image intensifiers no longer use a separate fluorescent screen. Instead, a cesium iodide phosphor is deposited directly on the photocathode of the intensifier tube. On a typical general purpose system, the output image is approximately 105 times brighter than the input image. This brightness gain comprises a flux gain (amplification of photon number) and minification gain (concentration of photons from a large input screen onto a small output screen) each of approximately 100. This level of gain is sufficient that quantum noise, due to the limited number of x-ray photons, is a significant factor limiting image quality.
Image intensifiers are available with input diameters of up to 45 cm, and a resolution of approximately 2-3 line pairs mm-1.
Flat-panel detectorsThe introduction of flat-panel detectors allows for the replacement of the image intensifier in fluoroscope design. Flat panel detectors offer increased sensitivity to X-rays, and therefore have the potential to reduce patient radiation dose. Temporal resolution is also improved over image intensifiers, reducing motion blurring. Contrast ratio is also improved over image intensifiers: flat-panel detectors are linear over a very wide latitude, whereas image intensifiers have a maximum contrast ratio of about 35:1. Spatial resolution is approximately equal, although an image intensifier operating in 'magnification' mode may be slightly better than a flat panel.
Flat panel detectors are considerably more expensive to purchase and repair than image intensifiers, so their uptake is primarily in specialties that require high-speed imaging, e.g., vascular imaging and cardiac catheterization.
Imaging concernsIn addition to spatial blurring factors that plague all x-ray imaging devices, caused by such things as Lubberts effect, K-fluorescence reabsorption and electron range, fluoroscopic systems also experience temporal blurring due to system lag. This temporal blurring has the effect of averaging frames together. While this helps reduce noise in images with stationary objects, it creates motion blurring for moving objects. Temporal blurring also complicates measurements of system performance for fluoroscopic systems.
Common procedures using fluoroscopy1.)Investigations of the gastrointestinal tract, including barium enemas, barium meals and barium swallows, and enteroclysis.
2.)Orthopaedic surgery to guide fracture reduction and the placement of metalwork.
3.)Angiography of the leg, heart and cerebral vessels.
4.)Placement of a PICC (peripherally inserted central catheter)
5.)Placement of a weighted feeding tube (e.g. Dobhoff) into the duodenum after previous attempts without fluoroscopy have failed.
6.)Urological surgery – particularly in retrograde pyelography.
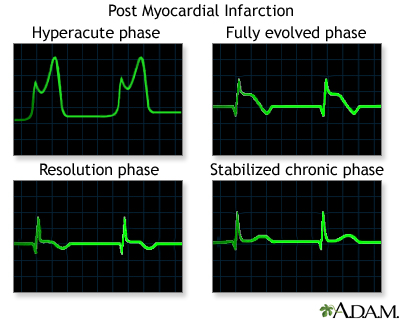
7.)Implantation of cardiac rhythm management devices (pacemakers, implantable cardioverter defibrillators and cardiac resynchronization devices)
Another common procedure is the modified barium swallow study during which barium-impregnated liquids and solids are ingested by the patient. A radiologist records and, with a speech pathologist, interprets the resulting images to diagnose oral and pharyngeal swallowing dysfunction. Modified barium swallow studies are also used in studying normal swallow function.
RisksBecause fluoroscopy involves the use of x rays, a form of ionizing radiation, all fluoroscopic procedures pose a potential health risk to the patient. Radiation doses to the patient depend greatly on the size of the patient as well as length of the procedure, with typical skin dose rates quoted as 20-50 mGy/min. Exposure times vary depending on the procedure being performed, but procedure times up to 75 minutes have been documented. Because of the long length of some procedures, in addition to standard cancer-inducing stochastic radiation effects, deterministic radiation effects have also been observed ranging from mild erythema, equivalent of a sun burn, to more serious burns.
A study has been performed by the Food and Drug Administration (FDA) entitled Radiation-induced Skin Injuries from Fluoroscopy with an additional publication to minimize further fluoroscopy-induced injuries, Public Health Advisory on Avoidance of Serious X-Ray-Induced skin Injuries to Patients During Fluoroscopically-Guided Procedures.
While deterministic radiation effects are a possibility, radiation burns are not typical of standard fluoroscopic procedures. Most procedures sufficiently long in length to produce radiation burns are part of necessary life-saving operations.
NOTES:
1.)ABSORBED DOSEAbsorbed dose (also known as Total Ionizing Dose, TID) is a measure of the energy deposited in a medium by ionizing radiation. It is equal to the energy deposited per unit mass of medium, and so has the unit J/kg, which is given the special name Gray (Gy).
Note that the absorbed dose is not a good indicator of the likely biological effect. 1 Gy of alpha radiation would be much more biologically damaging than 1 Gy of photon radiation for example. Appropriate weighting factors can be applied reflecting the different relative biological effects to find the equivalent dose.
The risk of stochastic effects due to radiation exposure can be quantified using the effective dose, which is a weighted average of the equivalent dose to each organ depending upon its radiosensitivity.
When ionising radiation is used to treat cancer, the doctor will usually prescribe the radiotherapy treatment in Gy. When risk from ionising radiation is being discussed, a related unit, the Sievert is used.
2.)
Specific absorption rateSpecific Absorption Rate (SAR) is a measure of the rate at which radio frequency (RF) energy is absorbed by the body when exposed to radio-frequency electromagnetic field. The most common use is in relation to cellular telephones. In the United States, the Federal Communications Commission (FCC) has adopted limits for safe exposure to RF energy produced by mobile devices and requires that phones sold in the U.S. have a SAR level at or below 1.6 watts per kilogram (W/kg) taken over a volume of 1 gram of tissue. In the EU the corresponding limit is 2 W/kg (averaged over ten grams of tissue).